Connect With Us

Arthritis Can Cause Pain in the Feet and Ankles
Symptoms of a Jones Fractures

Among the array of foot injuries, a Jones fracture demands rigorous attention. A Jones fracture, or avulsion fracture, occurs when a tendon or ligament forcefully pulls a small piece of bone away from the main bone. In the case of a Jones fracture, this typically occurs in the fifth metatarsal bone, which connects the pinky toe to the rest of the foot. This type of injury is often the result of a significant and direct impact, causing intense pain. Pain at the base of the foot is a primary symptom and should never be ignored, even if other symptoms are absent. Additionally, impaired movement of the little toe is common, though complete immobility may not always happen. Neglecting these symptoms can worsen the injury and may lead to surgery if the bone does not heal properly. Other signs to watch for with a Jones fracture can include impaired balance, swelling around the fifth metatarsal joint, and bruising around the little toe. Prompt medical attention from a podiatrist, including X-rays for accurate diagnosis and appropriate treatment, is essential for effective healing and preventing long-term complications. If you suspect a Jones fracture or are experiencing any of these symptoms, it is suggested that you schedule an appointment with a podiatrist for proper evaluation and care.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Deann Hofer Ogilvie, DPM from Ascend Foot & Ankle Center. Our practitioner can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Lafayette, CO . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
The human foot has 26 different bones, and the foot is divided into three parts: the hindfoot, the midfoot, and the forefoot. Each section of the foot is composed of a different amount of bones. For instance, the forefoot is made up of 19 bones. The midfoot is composed of five smaller bones called the navicular, cuboid, and three cuneiform bones. Lastly, the hindfoot is made up of only the talus and the calcaneus. The feet tend to be vulnerable to slipping and twisting; consequently, fractured bones within the foot are common. When a bone gets crushed, bent, twisted, or stretched it may become broken.
Many foot fractures occur through an accident or trauma. More specifically, common causes for broken feet are car accidents, falls, missteps, or overuse. If you have a broken ankle or foot, you may have one or more of the following symptoms: throbbing pain, swelling, bruising, tenderness, deformities, and difficulty walking.
There are some factors that may put you at a higher risk of developing a broken foot. People who participate in high-impact sports are more likely to develop foot fractures because of the stresses, direct blows, and twisting injuries involved in gameplay. Additionally, those who suddenly increase their activity level are more likely to suffer a stress fracture.
Unfortunately, there are different complications that may arise because of a foot fracture. For instance, arthritis may be caused by fractures that extend into the joints. Bone infections are also possible in open fractures due to the bone being exposed to bacteria. However, there are ways you can help prevent yourself from breaking your foot. One way to avoid fractures is to wear proper footwear. If you plan on going on a run, you should wear running shoes. You should also replace your shoes if you notice that they are becoming worn out. For runners, it is best to replace shoes every 300 to 400 miles.
Treatment for foot fractures usually consists of rest, ice, elevation, and compression (RICE). If you plan on wrapping your foot, try not to wrap it too tightly because doing so may cut off blood supply in the foot. You should also avoid walking on the fractured foot.
If you suspect you have a broken foot, you should see your podiatrist right away. It is important that you have someone bring you to your doctor, since driving with a broken foot can be dangerous. You should especially seek urgent care if you are experiencing numbness, pain, or deformities in your foot.
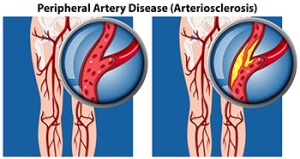
Understanding the Impact of PAD on Foot Health
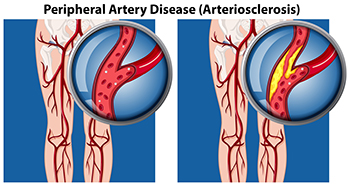
Peripheral artery disease, or PAD, is a prevalent vascular condition characterized by narrowed arteries that limits blood flow to the extremities (including the feet). The restricted blood flow deprives the feet of oxygen and vital nutrients, leading to a range of symptoms. Individuals with PAD may experience intermittent claudication, a condition marked by pain or cramping in the legs or feet during physical activity but subsides with rest. Other symptoms can include numbness, tingling, or weakness in the feet, particularly while at rest or during nighttime. As PAD progresses, individuals may develop non-healing wounds or ulcers on the feet, which pose a risk of infection and tissue damage. Recognizing the symptoms of PAD and seeking timely medical intervention is essential in managing the condition and preserving foot health. Regular exercise, smoking cessation, and medication management are among the strategies employed to lessen PAD's effects and improve overall vascular health. If you have tingling or numbness in your feet, it is suggested that you visit a podiatrist who can diagnose and help you to manage PAD.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Deann Hofer Ogilvie, DPM from Ascend Foot & Ankle Center. Our practitioner will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Lafayette, CO . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Complications of Peripheral Neuropathy
 Peripheral neuropathy results from damage to the peripheral nerves, which are responsible for sending information from the brain and spinal cord to the rest of the body. This condition often results in tingling, numbness, and pain in the affected areas, typically the hands and feet. Due to high blood sugar levels common in diabetes, people with this disease are more prone to peripheral neuropathy and the associated lack of sensation in the feet. This loss of feeling means that injuries, pressure sores, or other foot problems may go unnoticed. Without prompt and proper care, such untreated injuries can develop into diabetic foot ulcers, serious wounds that heal very slowly due to impaired circulation. If these ulcers become infected and treatment is not working, the ulcer can progress to gangrene, which involves the death of body tissue. This sometimes necessitates amputation to prevent further health complications. Regular check-ups with a podiatrist, or foot doctor, can help manage peripheral neuropathy and prevent severe complications. If you have peripheral neuropathy, it is suggested that you add a podiatrist to your regular care team.
Peripheral neuropathy results from damage to the peripheral nerves, which are responsible for sending information from the brain and spinal cord to the rest of the body. This condition often results in tingling, numbness, and pain in the affected areas, typically the hands and feet. Due to high blood sugar levels common in diabetes, people with this disease are more prone to peripheral neuropathy and the associated lack of sensation in the feet. This loss of feeling means that injuries, pressure sores, or other foot problems may go unnoticed. Without prompt and proper care, such untreated injuries can develop into diabetic foot ulcers, serious wounds that heal very slowly due to impaired circulation. If these ulcers become infected and treatment is not working, the ulcer can progress to gangrene, which involves the death of body tissue. This sometimes necessitates amputation to prevent further health complications. Regular check-ups with a podiatrist, or foot doctor, can help manage peripheral neuropathy and prevent severe complications. If you have peripheral neuropathy, it is suggested that you add a podiatrist to your regular care team.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Deann Hofer Ogilvie, DPM from Ascend Foot & Ankle Center. Our practitioner will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Lafayette, CO . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
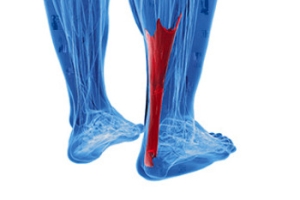
Exploring Achilles Tendonitis
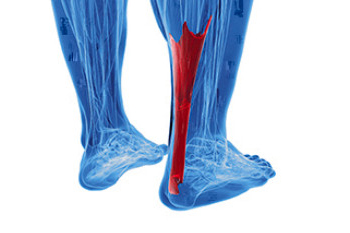
Achilles tendonitis is an ailment affecting the long tendon that connects the leg bones to the heel. This condition is particularly common among those engaged in high-impact activities, like running and jumping. The Achilles tendon's susceptibility to inflammation due to repetitive stress often leads to microtears and thickening. This results in Achilles tendonitis, which is characterized by posterior ankle pain and stiffness. However, the more severe consequence, an Achilles tendon rupture, typically occurs during forceful movements which result in sudden, intense pain and the inability to bear weight. Approximately 80 percent of Achilles tendon ruptures result in complete loss of function in the calf muscle. If you are experiencing pain in the Achilles tendon, it is suggested that you cease the activity causing the pain and make an appointment with a podiatrist as soon as possible. This foot doctor can conduct a thorough exam and determine the appropriate treatment.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Deann Hofer Ogilvie, DPM of Ascend Foot & Ankle Center. Our practitioner can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Lafayette, CO . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
How Smoking Can Affect the Feet

Beyond the well-known effects on your lungs and heart, smoking can also severely affect your feet, particularly through a condition known as Buerger’s disease. This disease targets the blood vessels in the arms and legs, causing swelling and reduced blood flow, which leads to the formation of clots. Consequently, individuals may experience pain, open sores or ulcers, and gangrene, which if not properly treated by a podiatrist may lead to limb loss. While the precise cause of Buerger’s disease remains uncertain, one undeniable link is tobacco use. Chemicals in tobacco irritate blood vessel linings, which then triggers inflammation and constriction. Nearly all diagnosed cases of Buerger’s disease are associated with tobacco use, whether through cigarettes, cigars, or chewing tobacco. Prevention is key, and that begins with quitting smoking and avoiding all forms of tobacco. But prioritizing your foot health is also essential, and by seeking guidance from a podiatrist you can manage symptoms and receive the needed wound care. If you're experiencing any symptoms, it is suggested that you make an appointment with a podiatrist for an exam and treatment.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact Deann Hofer Ogilvie, DPM from Ascend Foot & Ankle Center. Our practitioner will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact our office located in Lafayette, CO . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.