Connect With Us

Foot Problems in the Elderly

As we age, changes in foot structure can lead to common problems that affect mobility and comfort. Older adults may experience a loss of the fat pad under the foot, joint stiffness, decreased muscle strength, and flattening of the arch. These changes can cause foot pain, making daily activities more difficult. Foot pain in seniors is a significant concern because it increases the risk of falls and can alter a person’s walking pattern, leading to further issues with balance and stability. People with foot pain are also less likely to stay active, which can impact overall health. Common foot problems in older adults include arthritis, bunions, corns, calluses, and plantar fasciitis. Regular foot care, proper footwear, and conferring with a podiatrist can help manage these issues, improve comfort, and maintain mobility. If you are elderly or taking care of someone who is older and foot pain surfaces, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and appropriate treatment.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Deann Hofer Ogilvie, DPM from Ascend Foot & Ankle Center. Our practitioner can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in Lafayette, CO . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Elderly Foot Care
As you grow older, you will start to notice more problems with your feet due to wear and tear. This may also happen because the skin will start to become thin and lose elasticity. Some signs of aging feet are regular aches and pains, bunion development, and clawed toes.
Fortunately, there are ways you can improve comfort, relieve pain, and maintain mobility in your feet. One of the best ways to deal with aging feet is to exercise. If you keep active, your muscles will become toned which will then strengthen the arches in the foot and stimulate blood circulation.
It is important that you practice proper foot care to protect your aging feet. You should wash your feet in warm water on an everyday basis. Afterward, the feet need to be dried well and it is important to dry between the toes. Your toenails should be trimmed and kept under control; nails that are poorly cut may become ingrown. At the end of each day, performing an inspection of your feet will allow you to detect any ailments in their early stages.
As you grow older, it becomes more important that you wear comfortable shoes. Your shoes should be secure, and they should provide decent arch support. If you are looking to buy a new pair of shoes, it is best to look for a pair that are made from a breathable material. It is also helpful to have shoes that have a bit of extra room at the top of the shoe, especially if you suffer from swollen feet.
The most common foot problems that elderly people will encounter are bunions, calluses, corns, hammertoes, heel pain, and foot problems related to diabetes. Some other issues include arch pain, tarsal tunnel syndrome, Achilles tendonitis, and Morton’s neuroma
An annual foot examination is a great way for you to ensure that you do not have any serious health problems with your feet. You should talk to a podiatrist about the available treatment options for whichever foot issue you are dealing with.
Hyperhidrosis of the Feet
Hyperhidrosis of the feet, also termed plantar hyperhidrosis, is characterized by excessive sweating of the feet that can be onset by any cause, such as exercise, fever, or anxiety. Most people suffering from hyperhidrosis of the feet also experience hyperhidrosis of the hands, or palmar hyperhidrosis. Approximately 1-2% of Americans suffer from this disorder.
Sweating is a healthy process utilized by the body in order to cool itself and maintain a proper internal temperature, which is controlled by the sympathetic nervous system. In individuals with hyperhidrosis, the sympathetic nervous system works in "overdrive", producing far more sweat than is actually needed.
Plantar hyperhidrosis is considered primary hyperhidrosis. Secondary hyperhidrosis refers to excessive sweating that occurs in an area other than the feet, hands, or armpits, and this indicates that is related to another medical condition, such as menopause, hyperthyroidism, or Parkinson's disease.
Symptoms of hyperhidrosis of the feet can include foot odor, athlete's foot, infections, and blisters. Because of the continual moisture, shoes and socks can rot which creates an additional foul odor and can ruin the material, requiring shoes and socks to be replaced frequently. In addition to the physical symptoms, emotional health is often affected as this disorder can be very embarrassing.
If left untreated, hyperhidrosis will usually persist throughout an individual's life. However, there are several treatment options available. A common first approach to treating hyperhidrosis of the feet is a topical ointment. Aluminum chloride, an ingredient found in antiperspirants, can be effective at treating hyperhidrosis if used in high concentration and applied to the foot daily. Some individuals can experience relief this way, while others encounter extreme irritation and are unable to use the product. Another procedure is the use of Botulinum Toxin A, commonly referred to as Botox. This is injected directly into the foot, and is effective at minimizing the sweat glands in the injected area. These injections must be repeated every 4 to 9 months.
If these treatments are ineffective, oral prescription medications may be taken in an effort to alleviate the symptoms. Again, some will experience relief while others do not. Going barefoot reportedly provides relief for most sufferers.
A final approach to combating hyperhidrosis of the feet is through surgery. Surgery has been less successful on patients with plantar hyperhidrosis than on those with palmar hyperhidrosis. It is only recommended when sweating is severe and other treatments have failed to work. This kind of surgery usually involves going into the central nervous system, and cutting nerves to stop the transmission of signals telling the foot to sweat.
Treating Pain From Flat Feet

Flat feet, also known as fallen arches, occur when the arches of the feet collapse or are not properly developed. This condition can cause the entire foot to make contact with the ground while standing. Flat feet may be caused by genetics, injury, aging, or conditions like obesity and arthritis. Common symptoms include foot pain, particularly in the arch or heel, swelling, and discomfort during physical activities. Some people may experience knee, hip, or lower back pain due to the altered biomechanics of the body. Diagnosis typically involves a physical examination and imaging tests like X-rays to assess foot alignment. Treatment options range from wearing supportive footwear and custom orthotics to surgery for severe cases. While many people live comfortably with flat feet, untreated cases can lead to complications like tendonitis, arthritis, and chronic pain. If you have pain from flat feet, it is suggested that you consult a podiatrist for a diagnosis and pain-relieving treatment.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Deann Hofer Ogilvie, DPM from Ascend Foot & Ankle Center. Our practitioner will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Lafayette, CO . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a condition that occurs when the arches on the foot are flattened, which allows the soles of the feet to touch the floor. Flatfoot is a common condition and it is usually painless.
Throughout childhood, most people begin to develop arches in their feet, however, some do not. Those who do not develop arches are left with flatfoot. The pain associated with flat feet is usually at its worse when engaging in activity. Another symptom that may occur with those who have this condition is swelling along the inside of the ankle.
It is also possible to have flexible flatfoot. Flexible flatfoot occurs when the arch is visible while sitting or standing on the tiptoes, but it disappears when standing. People who have flexible flatfoot are often children and most outgrow it without any problems.
There are some risk factors that may make you more likely to develop flatfoot. Those who have diabetes and rheumatoid arthritis have an increased risk of flatfoot development. Other factors include aging and obesity.
Diagnosis for flat feet is usually done by a series of tests by your podiatrist. Your podiatrist will typically try an x-ray, CT scan, ultrasound, or MRI on the feet. Treatment is usually not necessary for flat foot unless it causes pain. However, therapy is often used for those who experience pain in their flat feet. Some other suggested treatment options are arch supports, stretching exercises, and supportive shoes.
Definition and Risk Factors of Sever’s Disease

Sever's disease, medically known as calcaneal apophysitis, is a common condition affecting children and adolescents, particularly those who are active in sports. Coined by Dr. Warren Sever in 1912, this condition involves inflammation of the growth plate at the heel, causing heel pain and discomfort. It typically occurs during periods of rapid growth when the Achilles tendon pulls on the developing heel bone. Risk factors for Sever's disease include engaging in high-impact sports, improper footwear, and participating in activities that involve frequent jumping or running. The condition is often characterized by pain and tenderness at the back of the heel, which can worsen with physical activity. If your active child has heel pain, it is suggested that you schedule an appointment with a podiatrist who can accurately diagnose and treat Sever’s disease.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Deann Hofer Ogilvie, DPM from Ascend Foot & Ankle Center. Our practitioner can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our office located in Lafayette, CO . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever’s disease, also known as calcaneal apophysitis is a common bone disorder that occurs during childhood. The disease is defined as an inflammation of the growth plate in the heel. When a child has a growth spurt, his heel bone grows faster than the muscles, tendons, and ligaments in his leg. This disease is a result of overuse. The people who are most likely to be affected by this disease are children who are in a growth spurt, especially boys who are from the ages of 5 to 13 years old. 60% of children with Sever’s disease have both heels involved.
Symptoms of this disease are heel pain that intensifies during running and jumping activities. The pain is typically localized to the posterior part of the heel. Symptoms may be severe, and they can easily interfere with daily activities. Children who play soccer, baseball, and basketball are more likely to develop Sever’s disease.
Your doctor will diagnose your child based on his or her symptoms, x-rays are generally not helpful in diagnosing this disease. Your doctor may examine both heels and ask your child questions about his or her activity level in sports. Your doctor may then use the squeeze test on your child’s heel to see if there is any pain. Nevertheless, some doctors might still use x-rays to rule out any other issues such as fractures, infections, and tumors.
Sever’s disease can be prevented by maintaining good flexibility while your child is growing. Another prevention method is to wear good-quality shoes that have firm support and a shock-absorbent sole. Sever’s disease can be treated by ceasing any activity that causes heel pain. You should apply ice to the injured heel for 20 minutes 3 times a day. Additionally, orthotics should be used for children who have high arches, flat feet, or bowed legs.
If you suspect your child has Sever’s disease, you should make an appointment with your podiatrist to have his or her foot examined. Your doctor may recommend nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen to relieve pain. In more severe cases, your child may need a cast to rest his or her heel. Fortunately, Sever’s disease does not cause long-term foot problems. After treatment, your child should start to feel better within two weeks to two months.
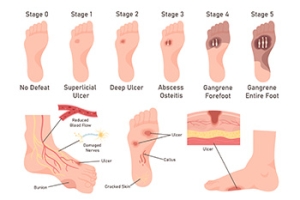
Diabetic Foot Ulcers Cause Foot Pain
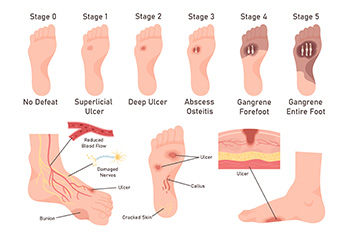
A diabetic foot ulcer is a serious complication of diabetes, characterized by a sore or wound on the foot that is slow to heal. These ulcers often develop due to poor blood circulation and nerve damage, common in diabetic patients. Risk factors include uncontrolled blood sugar levels, peripheral artery disease, and neuropathy, which diminishes sensation in the feet making injuries less noticeable. The progression of a diabetic foot ulcer typically begins with minor wounds or blisters that fail to heal properly. Over time, these can deepen and become infected, leading to more severe complications if not treated promptly. If you have developed a foot ulcer, whether or not it is related to diabetes, it is suggested that you are under the care of a podiatrist who can effectively treat this condition.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Deann Hofer Ogilvie, DPM from Ascend Foot & Ankle Center. Our practitioner will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Lafayette, CO . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.